Our guide helps organizations to develop the foundation for care management and assist those with a program to identify opportunities for improvement. Read the guide below or enter your email to download your copy to take on the go.

“Care management” is a broad framework that encompasses many different components, but they are all aimed at achieving a few very significant objectives: reduce health risks and the cost of care by delivering the most appropriate care to the most appropriate patients at the most appropriate times. Execution of effective care management isn't easy. It requires that organizations have a strong grasp of the needs of their patient populations and are capable of taking a team-based, patient-centered approach to treatment — one that must often be carried between sites of services and requires careful coordination of care transitions. But when care management is successful, it can transform an organization's delivery of care and services.
As with many healthcare initiatives, the more work an organization puts into its care management program, the greater the improvements it can expect to achieve. Of course, any efforts undertaken to develop and strengthen care management must be carefully executed to ensure there are no breakdowns in processes that can cause delay or harm patient care, prevent staff from performing at their full capacity, and waste valuable time and money.
This e-book aims to help organizations develop the foundation for care management, if they lack such a program, and assist those organizations with a program already implemented to identify a wide range of opportunities for improvement. It should represent just one of many resources organizations can use to help ensure their care management programs help deliver on the triple aim of healthcare: improving the experience of care, improving the health of populations, and reducing per capita costs of healthcare.
According to the last survey conducted by the U.S. Department of Health & Human Services, there were over 125 million outpatient department visits in a single year to U.S. hospitals. With such high patient volume, every healthcare organization should take a thorough review of its patient intake processes and identify areas for improvement. Here are a few best practices your organization should keep in mind when considering ways to improve your processes.
Address language and literacy — It’s essential to identify a patient’s preferred language and provide documentation in that language. If not, your patients may not understand your requests or feel comfortable completing required paperwork, which will make it more difficult to provide them care.
To ensure you’re prepared, have all documents in the common languages spoken in your community and a translator available. For organizations that can’t afford a full-time translator, there are several translation services and applications you can use.
Patients with low health literacy may also struggle to complete intake documentation. A screening process and a process for how to assist those patients should prove helpful.
Use EHR Module – Most electronic health record (EHR) systems include a standard module or offer an optional module to assist with patient intake. Before implementing these features, task those who will be working with the module to test it out and provide input. It’s also crucial to configure the intake module around your hospital’s specific needs.
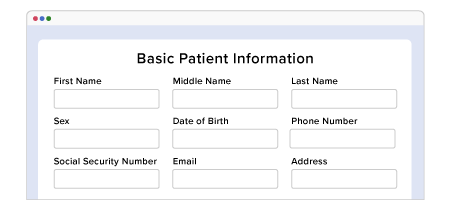
Invest in a Separate Management System – If your EHR’s intake functionality doesn’t adequately meet your organization’s needs, it may be beneficial to explore a patient intake management solution that can integrate with your EHR. Research has shown that using a patient intake management system can help organizations increase efficiency, focus more on the patient experience, and reduce overhead costs.

Leverage Electronic Messaging – To give patients the best care possible, providers must have access to detailed information, such as medication history, allergies, family history, information on primary care doctor, medical conditions, and history of hospitalizations. However, a major barrier to effectively gathering this information is that patients don’t always remember all these details.
Using electronic messaging provides the ability to remind patients through email and/or text that they should bring all medications to an appointment, undergo bloodwork, or come prepared to cover their portion of the payment.
If your institution does not use a messaging platform, there are several HIPAA compliant, secure messaging services you can research and consider (including Cureatr’s).

Monitor, Measure, Act — Finally, understanding that the patient intake process is critical to starting or continuing a patient’s treatment, you must also monitor and measure its performance. Make sure you’re also constantly seeking opportunities to improve performance and identifying potential problems. Tackle these issues and then continue to monitor and measure.

Another vital area of care management is patient engagement. Let’s take a look at three reasons why you should include patient engagement in your care management plan.
Enhancing Coordination of Care
While caregivers are largely responsible for care coordination, problems can arise if patients are not fully engaged and educated. A few potential problems with patients include:
Eliminate Duplication
If patients are asked to complete a particular service more than once, this could delay their treatment. In addition, it will also waste a patient’s money and a provider’s time and increase the potential risk of an investigation of fraud. To identify potential duplication, caregivers must ask patients whether they have already received a particular service when discussing treatment plans.
Help Patients More Effectively Manage Health Conditions
As Partners Healthcare notes:
“Evidence has shown that patients engaged in their health demonstrate improvements in their ability to self-manage their care, better outcomes and experiences in hospitals, and lower costs of care.”
Providers can help patients manage their own conditions by supporting them in the following ways:
Learn how patient engagement can help improve your care management program.
Care management programs have become a vital part of helping organizations improving the quality of care while reducing costs. They have become especially important as organizations have moved from fee-for-service to value-based payment models.
As you evaluate your care management program, consider these best practices.
There’s no easy solution for improving medication adherence and management. However, there are a few areas you can focus on that have a practical application and maximize the return on time invested.

Provide patients with fact sheets and tools — While putting together resources for patients may take some time in the beginning, it can be relatively inexpensive and worthwhile in the long run. If you don’t currently have such resources, look for information sheets online that can be used or modified.
In addition to pulling these together, designate a staff member who will be responsible for ensuring there are enough copies and that the information is kept current. It is worthwhile to consider providing these resources electronically via a patient portal or document repository and to have them available in many different languages.

Involve patients and families in the process — Clinicians can only do so much concerning medication management. By involving patients and their families, this will increase the likelihood of long-term adherence.

Fine-tune patient conversations —Clinicians have less time with patients than ever before. In fact, a USA Today article notes that some physicians who work for hospitals say they've been asked to see one patient every 11 minutes. With limited time to converse with a patient, this time must be used efficiently. For example, motivational interviewing is a patient-centered, non-confrontational communications skill set that can effectively drive patient conversations about medication issues and adherence. A valuable source for improving adherence conversations is the American Medical Association’s Steps Forward initiative.
Improving medication adherence and management in the outpatient setting requires a multi-faceted strategy that includes patient education, patient-clinician interaction, and patient engagement.
There are countless instances of patients going to the emergency room (ER) for non-emergency issues. Here are a few ways your organization can work to prevent unnecessary visits to the ER.
Gaps in care occur for many reasons. Often, when relationships between patients, providers, and payers develop problems, issues can then arise that allow patients to fall through the cracks of the system.
To avoid such scenarios, organizations should have actionable data at their fingertips. Here are a few steps to strengthen data collection and maximize its effectiveness.
Poorly coordinated care transitions waste billions of wasted annually. Poor transitions can also lead to poor health outcomes.
Care transitions are considered so important that there is a dedicated government initiative — the Community-based Care Transitions Program (CCTP) — that sets goals for improving care transitions for hospitals and other settings.
Let’s take a look at six recommendations for organizations to strengthen transitions:
Care transitions are a vital part of patient safety. Read the article to learn why.
Care coordination and care management are two important patient support services. To understand how coordination affects management, let’s look at the definitions of each concept.
This includes a combination of post-acute care needs and services across a variety of settings — from arranging for home health care or a skilled nursing facility to connecting patients with mental health, financial assistance, or durable medical equipment (DME) providers. Ultimately, this coordination exists to help patients and families navigate the complicated healthcare system.
Largely clinical and focused on delivering high-touch, post-acute care follow up as well as helping patients manage their medications, chronic conditions, and care needs. Typically delivered by nurses, care management is a team-based, patient-centered approach to reach out to and/or use technology to monitor patients. To deliver great care coordination that supports care management, consider these four recommended practices.
As you design your care management process, there are a few best practices to keep in mind.
To improve patient outcomes, there’s no better area to focus on than hospital workflows. Benefits of an improved workflow include:
To enhance your organization’s workflow, consider these four recommendations:
Focus on collaboration — Even just one individual who believes the workflow is flawed and performs a task differently than expected can affect the whole team and put patient safety at risk. This is why it’s vital to secure buy-in from all stakeholders, which may include department leadership, clinicians, IT representatives, staff, and vendors whose products and/or services are used in and support the workflow. While it is unlikely that buy-in will ever be unanimous, it is vital that organization leaders communicate the importance of the workflow and why following it is critical to patient safety and care.

Target challenging processes — Since some processes have a greater impact on patient safety than others, it’s essential to target these for assessment and improvement to help prevent negative outcomes. Some examples of processes to look at closely include:
Invest in technology — The right technology can make your organization’s processes more efficient. This may include clinical event notifications, workflow checklists, and task management solutions.
When searching for new technology to implement, it’s important that organizations do so carefully. Any new technology implementation is likely to affect your workflow, so do your due diligence prior to investing.


Do a redesign — Rather than making a series of changes across workflows, it may be necessary to start with brand new ones. This may be particularly helpful for processes or tasks being duplicated.
In a report by The Joint Commission on transitions of care, a study is referenced which estimates that 80% of serious medical errors involve miscommunication during hand-offs between medical providers.
Knowing that patient safety is at risk due to these errors, chief medical information officers (CMIOs) must make decisions based on data. Here are four statistics in particular that relate to improving care transitions.
“Falls often lead to devastating consequences; in fact, they represent the leading cause of injury-related death in those 65 and older. Hospital-based falls can be particularly problematic, with an estimated 30% resulting in serious injury.”
“… nearly 40% of patients are discharged with test results pending, and a comparable proportion are discharged with a plan to complete the diagnostic workup as an outpatient, placing patients at risk unless timely and complete follow-up is ensured.”
These are just a few revealing statistics that show the importance of CMIOs assessing the data captured by their organizations to determine what changes should be made to improve care transitions.
Decisions concerning care transition processes and technology investments made to support those processes must be driven by data, not anecdotes.
There are a few steps to consider as your organization works to reduce readmissions.
According to a Journal of Patient Safety study, about 13% of 30-day hospital readmissions occur due to adverse drug events (ADEs).
This statistic and other similar data points suggest that hospitals should focus on preventing medication mishaps to reduce readmissions. Here are three steps to focus on to help reduce 30-day readmits.
Learn 3 steps to preventing medication mishaps.
Post-hospital syndrome (PHS) is described as the temporary, vulnerable condition of patients after discharge that puts them at greater risk for generalized, adverse events that can cause readmission or death for reasons that have nothing to do with the condition for which they were being treated in the hospital.
While many patients may be readmitted due to poor discharge planning, mismanagement of medications, or lack of follow-up, inpatient stress may contribute to readmission more than organizations realize.
Below we’ll share a few ways hospitals can reduce the impact of stress and, therefore, readmissions that could be caused by PHS.
Enhance discharge post-acute care plans to address the effects of PHS
Make sure you explain PHS to patients and their families so they can watch for warning signs, which may include difficulty sleeping or anxiety. Providing written or electronic guidelines can also prove useful so that patients and their families can reference them and call their physicians, if needed.
Reduce unnecessary inpatient patient stressors
There are steps that providers can easily take to avoid stressors for patients. For example, work to eliminate some medical equipment noises and other unnecessary disturbances. It’s also important to ensure that you have enough staff to help patients when they need assistance. Don’t get caught up in following a process just because it has been in place for a while; modify process so that you are most effectively meeting patients’ needs.
Serve healthier, tastier food
If patients don’t want the food served in your hospital, this may disrupt their healing process as nutrition is an important element on the road to recovery. One great example is the Good Food, Healthy Hospitals Initiative in Philadelphia. Sixteen hospitals signed a pledge to offer healthier and more sustainable food and beverage options to patients, staff, and visitors.
Improve patients' surroundings
There are several steps hospitals can take to improve their patients’ surroundings. From providing rooms with cheerful colors and natural light to allowing patients to bring their own clothes rather than wear hospital gowns, even a seemingly minor detail can affect patients’ stress levels.
Be vigilant about follow-up
Finally, follow-up communication is a crucial step in helping patients avoid PHS. For example, patients may miss signs of a fever or mental health issue, which may be identified by a clinician communicating with them through a care management app, telehealth, or phone visit, or a visit by a home health provider. Follow-up calls should also inquire about patients’ well-being rather than just the condition for which they were in the hospital.
As we touched on earlier in this guide, the discharge planning process plays a key role in overall care management.
The idea of a seamless discharge planning process is simply when patients are effectively and safely transitioned from the hospital to their home. However, when seamless care does not happen, effects can include falls, adverse drug events, worsening conditions, or new, avoidable conditions.
A few effective ways to ensure a seamless discharge include:
So, what should be included in a hospital discharge summary? To start, let’s look at how this report from Advances in Patient Safety describes it:
“Hospital discharge summaries serve as the primary documents communicating a patient's care plan to the post-hospital care team. Often, the discharge summary is the only form of communication that accompanies the patient to the next setting of care. High-quality discharge summaries are generally thought to be essential for promoting patient safety during transitions between care settings, particularly during the initial post-hospital period.”
Here are the key components that should be included in a hospital discharge summary:
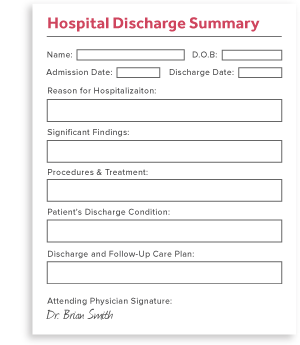
In addition to these essentials, a set of standards that came out of the Transitions of Care Consensus Conference (TOCCC) includes these elements:
It’s also important that post-discharge summaries are readily available for primary care physicians. Hospitals should consider ways they can improve the timeliness and availability of their summaries.
While patient discharge is an end to a patient's time in the hospital, it should not conclude care management, especially because poor discharge planning could lead to risks with patient safety and readmission.
For example, a classic study found that nearly 20% of patients experience adverse events within three weeks of discharge. As reducing readmissions becomes more important in care management, consider these four strategies to improve patient discharge.
When patients have longer wait times, they may be more susceptible to infection and other safety risks. Determine the length of your discharge wait times and assess your performance to identify ways to decrease these times.
Plan for discharge starting with admission rather than waiting until it’s time to release a patient.
Methods of engaging with patients can take many forms, but one of the best ways to improve engagement with discharge planning is to provide patients with a useful resource. One checklist that you can adapt for use in your facility is “Your Discharge Planning Checklist” from the Centers for Medicare & Medicaid Services.


Finally, by learning from the patient experience, you can work to improve areas where patient discharge might be weak. Survey patients to find out if they felt prepared for discharge and ask if any educational materials provided were helpful. Request any recommendations they might offer to improve the process.

An important part of strengthening discharge planning may include using the right tools. With so many resources available, we gathered five that we found interesting.
Learn five tools to improve care management.

For clinicians seeking additional resources to improve patient care, we compiled 13 apps we thought would be useful.
In addition to apps specific to patient care, there are even more healthcare mobile apps that can improve the quality and safety of care.
Medisafe
Medisafe’s founders created this app after their father accidentally took an extra dose of insulin and learned that similar situations happen often and end tragically. This app helps millions of patients take their medication on time and as prescribed.
Round Health
Round Health was founded by ex-Apple engineers and is similar to Medisafe, with features such as organizing the user’s medications and vitamins, setting up schedules and doses, and refill reminders. A unique feature is the app’s electronic medicine bottle, called Round Bottle. It offers automatic medication logging, performance tracking and insights, and caretaker notifications and alerts. It has GPS tracking, so it knows when users are away from the bottle, and also has a removal sensor to detect tampering.
TrekIT
A comprehensive platform, TrekIT is designed specifically for care coordination. It includes team-based task management functionality that helps improve clinical effectiveness. It was also designed using direct input from a wide range of users, including physicians, nurses, care managers, and clinical subject matter experts.
Wellth
Finally, Wellth is a health IT company based in Brooklyn, N.Y., that is working on providing a solution for medication non-adherence for chronic disease patients. Its Wellth app uses an innovative model incorporating behavioral economics and technology. Patients are offered an amount of money to take their medication for a specified amount of time. Using the app to verify adherence, patients take a picture of the medication in their hand. A penalty is applied each time patients fail to take their medication. Wellth states that this model has helped reduce readmission for their clients by 40% or more.
While you may have reached the end of this e-book, your work has only just begun. Now comes the hard part. It's time to implement what you’ve learned so you can create a care management program that delivers significant, measurable improvements in your quality of service or further strengthen a program that is likely already helping you provide high-quality, cost effective care.
Do you feel like you already have a pretty good care management program? That's terrific. But ask yourself: Would you settle for satisfactory care or would you want exceptional care? Apply that to your care management program. Can it be better? And if it can, shouldn't it be? That needs to be the mentality that drives any care management program. Apply the guidance from this e-book and other valuable care management resources you have come across and strive to turn good processes into great ones. Share these resources with the various areas of your organization that would benefit from the recommended practices provided within them. Bring together stakeholders and program champions and work to make meaningful changes.
As you do, measure and monitor them to ensure they are having their desired effects. If results come up a little short, that's okay. You can find some satisfaction in improvements of any size — after all, even a small improvement can have a significant impact on the patient experience. Then keep working to achieve bigger enhancements and see how they affect an even larger portion of your patient population. Know that such gains are possible for any care management program. By maintaining an unwavering commitment to the building blocks of care management — a team-based, patient-centered approach to care — and a desire to truly transform your delivery of care, you may be surprised how quickly your efforts begin to positively impact the lives of your patient populations.
 Save this information for later.
Save this information for later.
© Cureatr 2023 | Privacy Policy
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).